EQuiP, the European Society for Quality and Safety in Family Practice, one of the WONCA Europe networks, organized its open Spring meeting 2013 in Paris on the topic of Equity in primary health care. At the same time a Working Group on Equity was formed aiming to keep the debate on equity in the network ongoing and to ensure the theme of equity is considered in the activities of EQuiP involving the other dimensions of quality. This consensus statement is the result of a series of debates and workshops organized during EQuiP and Wonca conferences and meetings between 2013 and 2017.
Please download the EQuiP Position Paper on Equity - a core dimension of Quality in Primary Care (PDF) here.
#1 EQuiP recognizes equity as an essential dimension of quality of health care, as are, effectiveness, efficiency, safety, timeliness, and patient centredness.
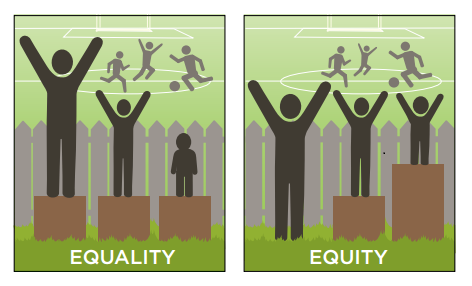
Equitable health care is hereby considered as health care in which the access to care, treatment, and outcome of care do not vary according to any patient characteristic different than his/her health needs. Enhanced health services should be provided where greater health needs are present (vertical equity). No differences in health services should occur where health needs are equal (horizontal equity).
#2 EQuiP advocates that equity should be one of the core principles to guide practice organization and care processes in primary care.
#3 Enhancing equity in primary health care asks not only for actions that tackle financial barriers to health care but also for actions that guarantee the availability and acceptability of care for all patients.
EQuiP supports the call for universal health care to ensure that all people can use the promotional, preventive, curative, rehabilitative and palliative health services they need, while not exposing the user to financial hardship when doing so.
EQuiP also stresses the importance of tackling non-financial barriers by ensuring a fair geographical distribution of high quality health care facilities and medications; the availability of staff with the right skills in the right place and of well-equipped facilities within easy reach; and of services acceptable for all patients and patient groups. (With this statement EQuiP endorses the report of the European EXPH on Access to health services in the European Union).
#4 Primary care providers should assess patients’ socioeconomic, demographic cultural and other relevant characteristics. This allows health care to be adjusted to patients’ specific health needs. If this patient information is recorded in the patient’s medical file, this has to be done with the patient’s consent and with respect for the privacy of the patient and the confidentiality of the information.
The benefits of recording these characteristics should outweigh any risks of discrimination. Under no condition should this information be used to deny medical care or provide medical care of lower quality to patients because of their demographic, socio-economic or ethnic background.
#5 EQuiP strongly advises primary care professionals and practices to evaluate the equity of the care they deliver, and undertake practice–based quality improvement initiatives which incorporate the aim of improving equity of health care.
This evaluation can include analyzing equity in performance indicators (e.g. vaccination rate, patient satisfaction), but also critical incident analysis and self-evaluation of staff. Information from an equity assessment should be used to tailor care process to the needs of the patients as delivering the same care to all patients equals inequity in care.
#6 EQuiP asks that health authorities support primary care professionals delivering equitable care and that the level of support is according to the assessed level of need of the population served. This support can include increased financial rewarding e.g. compensating the additional time and practice resources invested when delivering equitable care; instrumental support e.g. diversity-sensitive patient education materials; and information support e.g. continuous medical education programs on equity related topics.
In the decision making process on support strategies primary care professionals knowing the day-to- day reality of working in deprived areas and/or with vulnerable population groups should be involved in order to match the actions undertaken to the needs of practices and providers.
#7 EQuiP recognises interprofessional collaboration as a key strategy in the delivery of equitable health care, with most to gain for patients with complex care needs.
By bringing together the expertise of health and social professions, both in primary and specialist care, and by a better coordination of care, the health and social needs of the patients can be met in a comprehensive way. The organisation of the interprofessional collaboration needs to be taylored to the specific context in order to optimize the opportunities and available resources.
#8 EQuiP endorses the international call for proportionate universalism in the action against health inequity: the resourcing and delivering of universal services at a scale and intensity proportionate to the degree of need.
#9 EQuiP recognizes community oriented primary care as a strategy to tackle the social determinants of health by identifying the priority health needs of the community and developing and implementing interventions addressing these in partnership with community members, patients and stakeholders.
#10 EQuiP strongly advises that all primary care professionals are trained in the importance of the social determinants of health, community oriented care, dealing with diversity, and interprofessional collaboration. This should be further strengthened in continuous professional development programs.
#11 Primary care professionals should take up the advocacy role not only for individual patients but also for patients groups and populations as they are witnesses of the social conditions in which people live and work, of inequity in the health care system and of health inequities.
Position Paper prepared by the EQuiP Equity Working Group and accepted by the EQuiP General Assembly during the Zagreb Meeting on 18/11/2017.
Published on 15 December 2017.